Ever been told your knee or hip pain could be a result of your feet?
Ever heard from a physiotherapist or a personal trainer that your “local pain” could be “coming from elsewhere”? Common rhetoric includes that your shoulder might be hurting because of your tight upper spine or back, that your low back pain might be coming from your weak core, or that your knee or hip pain might be coming from your feet (ground-up approach). Is this true, and how can one area of the body have an effect on another part of the body?
How can one area of the body impact another area?
Yes, movement or stress at one area of the body can have an impact on the rest of the body. Just think when you’ve stubbed your toe. If you stub your right toe, you typically start limping and fully weight the left leg, seize up at your right hip and knee, and your whole gait changes. Similarly, when you break your arm and get a cast or a sling, your whole upper body posture changes, and sometimes you even feel like you need a back massage after some time!
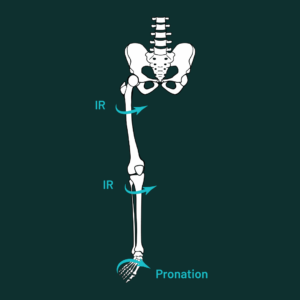
Similarly at the foot, , even in an uninjured state, when you start by standing on two feet, and you pronate them both as much as you can (push into the inside pressure of the foot), you’ll notice that the knees naturally come along for the ride and drop inwards, your hips follow suit, and you might even notice your belly wanting to push forward or your low back start to extend. Here is a demonstration:
What does the research say about it?
While there is quite a bit of research on the foot, there is a large proportion of research done statically rather than dynamically. But, when most of us use our feet, we are using them in a dynamic way, either simply to support our body weight when standing, or for locomotion (walking and running). The question about whether or not the foot has upstream effects on the rest of our biomechanics is a hot topic because if it can have a negative effect on mechanics, there could be potential injuries that we would be inclined to try to prevent.
Foot pronation is a triplanar motion – meaning it occurs technically-speaking in 3 planes: Rear foot eversion, forefoot abduction, and ankle dorsiflexion. In more simple terms, if a lay-person were looking at the foot and describing the motion when pronation occurs – they would describe the inside pressure of the foot being more close to the ground (as in flat feet) or on more of the big toe pressure. Since flat foot has been associated with musculoskeletal disorders such as medial tibial stress (2), patellofemoral pain (4), or low back pain (3), learning more about how these shapes contribute to upstream mechanics is of interest to researchers.
The research by Dodelin et al (2020) seeked to determine whether foot pronation would change lower limb mechanics during gait. They recruited 295 firefighters between the ages of 20 and 50 years old. They were measured during barefoot gait of a self selected speed with a 3D motion capture system.
From their research they found that those who were categorized as pronators (aka: pronated past a certain angle during ambulation), had alterations in their lower limb and foot kinematics during gait. These alterations included more knee internal rotation (knee collapses inwards), hip adduction (when the swing leg hip collapses and the pelvis drops towards the standing leg), and although their study did not find increases in anterior pelvic tilt (low back extended position, in lay-terms), previous studies had found that anterior pelvic tilt indeed did increase in pronated feet (5). They found, as expected, that in the conditions where the subjects pronated the most, the pressure on the outside of their foot was the lowest.
Similarly to this sketch of the lower body, when the foot collapses, it can have the tendency to pull the knee and hip inwards with it (into internal rotation aka IR).
So can feet change knee and hip injury risk?
From that research, the group concluded that, “Foot pronation might increase the risk of pathology in the lower limb joints and muscles. Increased forefoot abduction (which is essentially when the top part of your foot has the most pressure on the big toe and the least on the little toes) has recently been reported as a predictive factor for lower limb musculoskeletal (MSD) disorders.”
To clarify, musculoskeletal disorders (MSD) are injuries or disorders of the muscles, nerves, tendons, joints, cartilage, and spinal discs. In the world of physiotherapy and kinesiology, we might define conditions our athlete or client have, to use appropriate protocols for rehab.
Some examples are:
- Carpal tunnel syndrome.
- Tendinitis (acute/inflammatory) or tendinosus (chronic)
- Patellofemoral pain (pain in the knee)
- Plantar fasciitis
- Rotator cuff injuries (affects the shoulder)
- Epicondylitis (affects the elbow)
- Tennis elbow
- Muscle strains and low back injuries
- Unspecific hip, knee, or foot pain
- Flat feet, bunions, and other foot issues
If the way that we walk or run, then, can have an effect on some of the injuries and MSD’s we are at risk of getting, the way we walk or run might be important.
Further into the conclusions of the same study by Dodelin et al (2020):
“This study has important clinical implications relating to the understanding of both foot and lower limb movement in individuals with pronated foot-function.,, The results suggest that individuals with pronated foot-function, though asymptomatic, may have a greater risk of lower limb MSD due to the increase in forefoot abduction…. In addition, the increase in forefoot dorsiflexion in the [foot pronation example] is a mechanism for foot collapse when the foot is in a flat position on the ground…. Strengthening of the intrinsic foot muscles could limit this phenomenon and could be a useful injury prevention strategy in asymptomatic pronators. Finally…. pronated foot-function could alter lower limb and pelvic kinematics and increase constraints on the knee and the lumbar region (low back/hip region). We therefore suggest that foot-function should be evaluated as part of a holistic assessment in the case of knee injury or low back pain.”
So per this research, and similarly what we seem to find when we assess individuals for training (often runners or athletes who play sports that involve running or cutting), these patterns of foot problems do seem to have clear effects on their upstream movement and mechanics.
Can strengthening or training the feet have an impact on the knee and hip?
Some researchers have reported that weak hip external rotators of the hip (commonly referred to as the glutes) internally rotates the hip joint (causes thigh to rotate inwards) while inducing foot pronation (causes foot to press down into the big toe and arch side). The results of one study showed that as the activity of the abductor hallucis muscle increased (the muscle responsible in pulling the big toe away from the other toes), the arch drop decreased, indicating that even this type of isolated foot exercise could be helpful for the maintenance and enhancement of the arch (7).
In a study of various exercises for strengthening the big toe, toe-spread exercises and short-foot exercises performed in the sitting position did not elicit any significant difference in the abductor hallucis muscle activity, but the muscle activity value was shown to be higher during the toe-spread exercises (10). So, even non-weight bearing foot strength exercises can be valuable for strengthening the foot and preventing arch collapse and pronation.
It does appear, therefore, that a valgus stress (inwards motion with excessive inside pressure on the kne) is created in the knee joints during gait as a result of pronation and the internal rotation of the lower extremities, leading to kinematic sway of the lower extremities and compensatory actions (8).
Based on these and other study’s results, hip external rotator (glutes, put simply) muscle strengthening is considered to have effects on preventing navicular drop and arch collapse in people with lots of pronation at the foot (8).
What to look for in your Foot Strength Program
We tend to be very critical of the way that foot injuries are currently treated because we have had too many clients come to us saying they were referred for injections, xrays, and surgeries without anyone even evaluating their movement! To be 100% clear – we are a team of Strength and Conditioning, Exercise Physiology, Kinesiologists, and Athletic Therapists. Besides our athletic therapists, we typically work more on the training and strength side of things than in the clinic. With that being said, we are referred athletes and clients from many physiotherapists chiropractors, and the like, and so rehabbing and getting people out of pain comes as part of our jobs.
With the experiences we’ve had with rehabilitation of many foot, knee, hip, and other injuries and issues, so many people are ONLY given passive solutions to these things. Of course there are instances when all of those modalities are suitable, but when people are left to “rest”, “get a massage”, or something else that is passive, and the condition doesn’t improve – often the next step is that they get referred to more extreme treatments (like surgery and injections). Often – strength, control, and mobility, we’ve found, can go a VERY long way in preventing future injections and surgeries – or in the very least delaying them as long as possible. Something really has to change.
That is why we created the Foot Foundations program. It is an 8-week program designed to give you the tools to evaluate your foot strength and mobility, and then progress through 8 weeks and 3 different training phases of food and ankle specific training. We don’t know of a single program as comprehensive as ours for a few reasons:
- Most of the time, if you’re lucky, you might get prescribed calf raises for an ankle issue. News flash, the calves aren’t the only muscles we need for the strongest and most resilient feet and ankles!
- For that reason, foot intrinsic strength is key too. Foot intrinsic muscles are the ones that connect to bones in the foot, but that don’t cross the ankle joint like the calf does through its attachment to the achilles and heel. But, news flash again, foot scrunches are not adequate for training all of the foot intrinsic muscles
- More often than not, all people are prescribed foot orthotics or to “stay off their feet” but this doesn’t do anything for foot strength or mobility. Orthotics can actually make the foot muscles shrink (Protopapas & Perry, 2020).
Check Out Our Foot Foundations Program that we created specifically for foot problems, but that transfer to knee and hip issues as well.
References:
- Dodelin, D., Tourny, C., & L’Hermette, M. (2020). The biomechanical effects of pronated foot function on gait. An experimental study. Scandinavian Journal of Medicine & Science in Sports, sms.13785. https://doi.org/10.1111/sms.13785
- Moen MH, Bongers T, Bakker EW, Zimmermann WO, Weir A, Tol JL, Backx FJG. Risk factors and prognostic indicators for medial tibial stress syndrome. Scand J Med Sci Sports 2012;22:34–39.
- Kosashvili Y, Fridman T, Backstein D, Safir O, Ziv YB. The Correlation between Pes Planus and Anterior Knee or Intermittent Low Back Pain. Foot Ankle Int 2008;29:910–913.
- Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain:proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther 2012;42:A1-54.
- Protopapas, K., & Perry, S. D. (2020). The effect of a 12-week custom foot orthotic intervention on muscle size and muscle activity of the intrinsic foot muscle of young adults during gait termination. Clinical Biomechanics, 78. https://doi.org/10.1016/j.clinbiomech.2020.105063
- Tateuchi H, Wada O, Ichihashi N. Effects of calcaneal eversion on three-dimensional kinematics of the hip, pelvis and thorax in unilateral weight bearing. Hum Mov Sci 2011;30:566–573.
- Goo, Y.-M., Kim, D.-Y., & Kim, T.-H. (2016). The effects of hip external rotator exercises and toe-spread exercises on lower extremity muscle activities during stair-walking in subjects with pronated foot. J. Phys. Ther. Sci. , 28, 816–819.
- Neumann DA: Kinesiology of the musculoskeletal system: Foundations for rehabilitation, 2nd ed. Missouri: Mosby,2010.
- Tome J, Nawoczenski DA, Flemister A, et al.: Comparison of foot kinematics between subjects with posterior tibialis tendon dysfunction and healthy controls. J Orthop Sports Phys Ther, 2006, 36: 635–644.
- Nyland J, Kuzemchek S, Parks M, et al.: Femoral anteversion influences vastus medialis and gluteus medius EMG amplitude: composite hip abductor EMG amplitude ratios during isometric combined hip abduction-external rotation. J Electromyogr Kinesiol, 2004, 14: 255–261.
- Heo HJ, An DH: The effect of an inclined ankle on the activation of the abductor hallucis muscle during short foot exercise. J Phys Ther Sci, 2014, 26: 619–620.
- Hashimoto T, Sakuraba K: Strength training for the intrinsic flexor muscles of the foot: effects on muscle strength, the foot arch, and dynamic parameters before and after the training. J Phys Ther Sci, 2014, 26: 373–376.
- Jung DY, Kim MH, Koh EK, et al.: A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys Ther Sport, 2011, 12: 30–35
- Kendall FP, McCreary EK, Provance PG, et al.: Muscles: Testing and function with posture and pain, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 2005
- Hoving, J., de Vet, H., Koes, B. W., van Mameren, H., Deville, W., van der Windt, D., Assendelft, W., Pool, J., Scholten, R., Korthals-De Bos, I, & Bouter, L. (2006). Manual Therapy, Physical Therapy, or Continued Care by the General Practitioner for Patients With Neck Pain. Physical Therapy, 22(4), 370–378.